Summary
Cardiogenic shock (CS) represents a heterogeneous clinical syndrome characterized by sustained tissue hypoperfusion due to cardiac dysfunction, encompassing diverse etiological, hemodynamic, and molecular profiles. The paper emphasizes the need for recognizing CS heterogeneity through clinical classification, ventriculo-arterial coupling, macro- and microcirculatory considerations, and molecular subphenotyping. These multiple layers of complexity suggest that personalized medicine strategies, including advanced physiological monitoring and biomarker-guided interventions, could significantly improve outcomes for CS patients.
Key Points:
- Definition and Clinical Classification: Cardiogenic shock is defined as a cardiac-related condition leading to prolonged tissue hypoperfusion despite adequate intravascular volume, classically manifested by hypotension, low cardiac output, and clinical signs of impaired organ perfusion. Classification includes acute myocardial infarction-induced shock (AMI-CS), heart failure-related CS (HF-CS), secondary CS from arrhythmias or valvular issues, and post-cardiotomy CS.
- Shock Severity Heterogeneity: The updated SCAI (Society for Cardiovascular Angiography and Interventions) classification, widely accepted, integrates clinical, biochemical, and hemodynamic variables to categorize shock severity, aiding prognostic prediction and clinical decision-making regarding interventions such as mechanical circulatory support.
- Ventriculo-Arterial (V–A) (Un)coupling: Effective interaction between ventricular function and arterial load, termed V–A coupling, is crucial for optimal perfusion. In CS, disturbances in ventricular elastance (Ees) and arterial elastance (Ea) cause V–A uncoupling, critically affecting cardiac efficiency and perfusion pressure, thus guiding tailored therapeutic strategies.
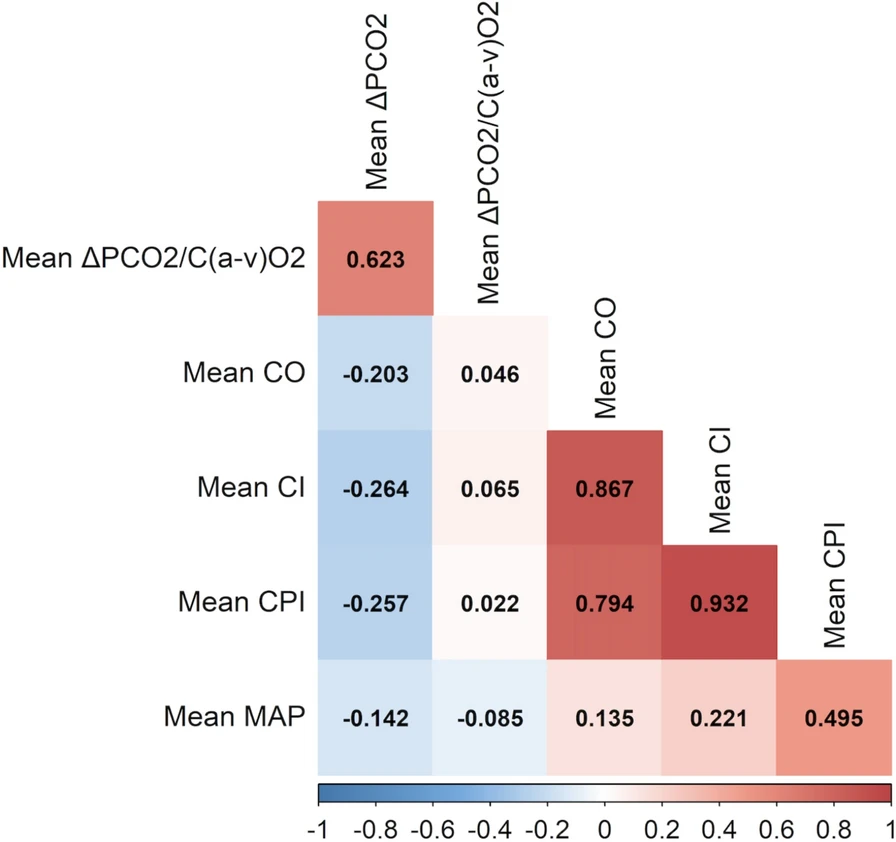
- Macro/Microcirculatory Uncoupling: Standard macrohemodynamic targets (blood pressure, cardiac output) often inadequately represent microcirculatory function. Persistent microcirculatory dysfunction—despite optimal macrohemodynamics—is common in CS, manifesting as microvascular thrombosis, endothelial dysfunction, or tissue edema, necessitating more nuanced bedside monitoring techniques.
- Molecular and Biological Heterogeneity: Molecular subphenotyping, employing advanced techniques such as unsupervised machine learning, has identified distinct CS subphenotypes characterized by differential expressions of biomarkers related to endothelial dysfunction, inflammation, and myocardial injury, each correlating independently with mortality.
- Clinical Implications of Subphenotyping: Utilizing clinical, physiological, and molecular subphenotypes facilitates personalized treatment approaches, better trial designs, and improved patient stratification for targeted therapies. Examples include studies assessing interventions like the Impella device and adrecizumab, illustrating how subphenotype-based selection might impact clinical trial outcomes.
- Integration of Advanced Monitoring: Incorporating continuous and advanced monitoring techniques—such as echocardiography, waveform analysis, microcirculatory monitoring, and multi-omics biomarkers—enhances comprehensive physiological and pathological characterization of CS, supporting precise clinical management.
- Microcirculation as a Therapeutic Target: Clinical trials exploring interventions aimed at improving microcirculatory function have demonstrated biological plausibility, although achieving meaningful clinical benefits remains challenging. Future studies targeting microcirculatory dysfunction are suggested, particularly in patients with optimal macrohemodynamics.
- Potential Role of Machine Learning: The application of machine learning methods offers promising avenues for identifying clinically meaningful subphenotypes of CS patients. Such technologies could refine prognosis, guide interventions, and support the delivery of precision medicine in CS management.
- Precision Medicine and Future Directions: Precision medicine approaches, exemplified by initiatives such as ShockCO-OP, integrate multiple clinical, physiological, and biomolecular data streams, demonstrating feasibility in personalized management of CS. This paradigm shift aims to address inherent heterogeneity, optimize patient outcomes, and guide future research.

Conclusion
Cardiogenic shock encompasses significant heterogeneity across clinical, hemodynamic, and molecular dimensions, complicating management strategies. Adopting sophisticated, integrative approaches—including physiological monitoring, molecular profiling, and advanced analytics—can better define subphenotypes and personalize treatment, ultimately improving outcomes and shaping future therapeutic innovations.

Discussion Questions:
- How can critical care teams practically integrate comprehensive subphenotyping strategies into real-time clinical decision-making for cardiogenic shock?
- What are the most promising avenues of research to translate insights from molecular and microcirculatory subphenotypes into actionable clinical therapies?
- Given the complexity and resource demands of personalized medicine in cardiogenic shock, how can healthcare systems effectively implement these strategies to balance precision with feasibility?
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.