Abstract:
Jung et al. provide a comprehensive review addressing current knowledge and contemporary practices in the management of cardiogenic shock (CS). Despite advancements, mortality remains high, and the complexity of patient care underscores the need for individualized treatments. The authors highlight recent evidence in pharmacological therapies, mechanical circulatory support (MCS), and the potential for personalized medicine facilitated by advanced biomarkers and artificial intelligence.

Key Insights:
- Definition and Classification: CS is clinically defined as end-organ hypoperfusion caused by inadequate cardiac output despite sufficient intravascular volume, commonly identified by hypotension and elevated filling pressures.
- Epidemiology and Mortality: Despite improved therapeutic approaches, mortality in cardiogenic shock remains consistently high (approximately 40–50% in acute myocardial infarction-related CS), highlighting the need for more effective strategies.
- Pathophysiology and Clinical Phenotypes: CS involves a cascade starting with reduced cardiac output and elevated filling pressures, progressing to systemic inflammation and multiorgan dysfunction, requiring rapid intervention to interrupt this downward spiral.
- Traditional vs. Emerging Classification: The authors discuss the traditional hemodynamic approach versus the Society for Cardiovascular Angiography and Interventions (SCAI) shock severity staging system, emphasizing the benefits of more nuanced stratification for clinical management and research.
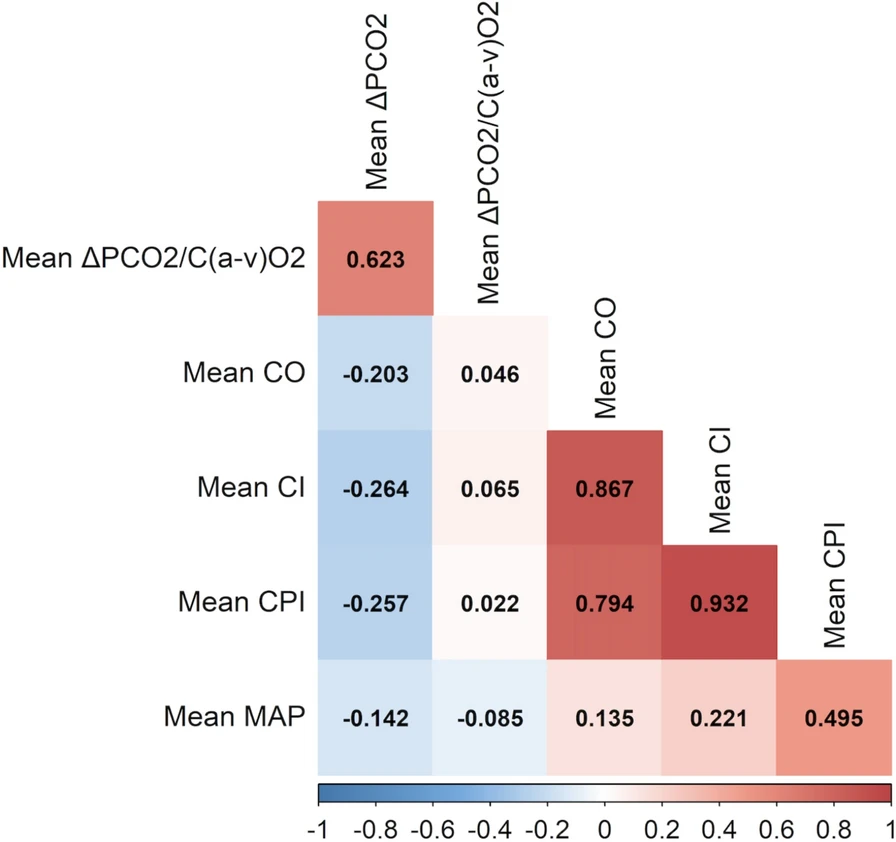
- Diagnostic and Monitoring Tools: Effective management relies on continuous monitoring, including invasive arterial pressures, central venous pressures, pulmonary artery catheterization, echocardiography, and biomarkers such as lactate, NT-proBNP, and troponins.
- Pharmacological Treatment: Pharmacologic interventions focus on optimizing preload (fluid management), afterload (vasopressors like norepinephrine), and contractility (inotropes like dobutamine and levosimendan), though definitive evidence supporting their superiority remains limited.
- Mechanical Circulatory Support (MCS): Temporary mechanical support devices (e.g., ECMO, Impella, intra-aortic balloon pump—IABP) offer critical hemodynamic support in refractory cases, yet recent randomized controlled trials have shown mixed results regarding their impact on survival.
- Challenges in Clinical Trials: Conducting high-quality trials in CS is inherently challenging due to heterogeneity in patient populations, rapidly evolving clinical status, and ethical considerations, resulting in limited definitive evidence for many common interventions.
- Future Directions and Innovations: Future management strategies may integrate advanced biomarker-driven phenotyping and artificial intelligence to define specific patient endotypes, thereby enabling tailored therapeutic approaches and improved outcomes.
- Resource Allocation and Cost-Effectiveness: The authors highlight the significant resource utilization and economic burden associated with CS, emphasizing the potential benefits of protocolized management and specialized multidisciplinary shock teams to reduce costs and improve patient outcomes.

Conclusion: The current state-of-the-art management of cardiogenic shock involves a comprehensive yet challenging approach, with ongoing high mortality rates despite advancements in pharmacological and mechanical support therapies. Moving towards personalized medicine through enhanced patient phenotyping, biomarker integration, and advanced analytics may represent the future of effective CS management.
Watch the following video on “Cardiogenic Shock Virtual Grand Rounds: Cardiogenic Shock Systems of Care” by American Heart Association
Discussion Questions:
- How can biomarker-driven patient stratification practically be integrated into daily clinical management of cardiogenic shock?
- What steps are needed to standardize and optimize the use of mechanical circulatory support devices in different clinical settings?
- What should be prioritized in future clinical trials to better define effective interventions and improve survival outcomes in cardiogenic shock?
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.