Summary
Hemorrhagic shock remains a leading cause of preventable death globally, characterized by a complex, time-sensitive inflammatory response that evolves from hyperinflammation to immunosuppression. This review explores the pathophysiology, progression, and systemic consequences of hemorrhagic shock, emphasizing the interplay between tissue injury, endothelial dysfunction, coagulopathy, and metabolic derangements. The article outlines established and emerging biomarkers, evaluates current and investigational therapies, and highlights the critical importance of tailored, phase-specific interventions to improve patient outcomes. Future directions center on precision medicine, real-time monitoring, and coordinated care strategies to overcome both biological and systemic challenges.
Key Points:
- Temporal Pathophysiology of Hemorrhagic Shock: Hemorrhagic shock progresses through an initial hyperinflammatory response followed by immunosuppression, marked by complex interactions between tissue damage, endothelial activation, and systemic cytokine signaling.
- Shock Classification and Clinical Impact: Classification into Classes I–IV correlates with increasing blood loss and systemic dysfunction, where Class III and IV hemorrhages trigger severe inflammation, coagulopathy, and rapid multi-organ failure without intervention.
- Endothelial Dysfunction and Glycocalyx Shedding: Vascular endothelial cells play a pivotal role in mediating shock response, with glycocalyx degradation (indicated by elevated syndecan-1) leading to vascular leakage, inflammation, and coagulopathy.
- Gut Barrier and Systemic Inflammation: Splanchnic ischemia during early shock impairs gut integrity, allowing bacterial translocation and systemic dissemination of inflammatory mediators, contributing to multi-organ dysfunction.
- Oxidative Stress and Mitochondrial Dysfunction: Cellular damage is exacerbated by ROS produced during hypoperfusion, leading to DNA injury, impaired metabolism, and further immune activation, particularly through NADPH oxidase pathways.
- Coagulopathy in Trauma: Trauma-induced coagulopathy varies with injury pattern; penetrating trauma often causes dilutional coagulopathy, while blunt trauma leads to disseminated intravascular coagulation driven by endothelial activation and tissue factor release.
- Transition to Immunosuppression: A distinct compensatory anti-inflammatory response syndrome (CARS) emerges within days post-injury, characterized by reduced monocyte HLA-DR expression, lymphocyte apoptosis, and expansion of regulatory T cells, increasing infection susceptibility.
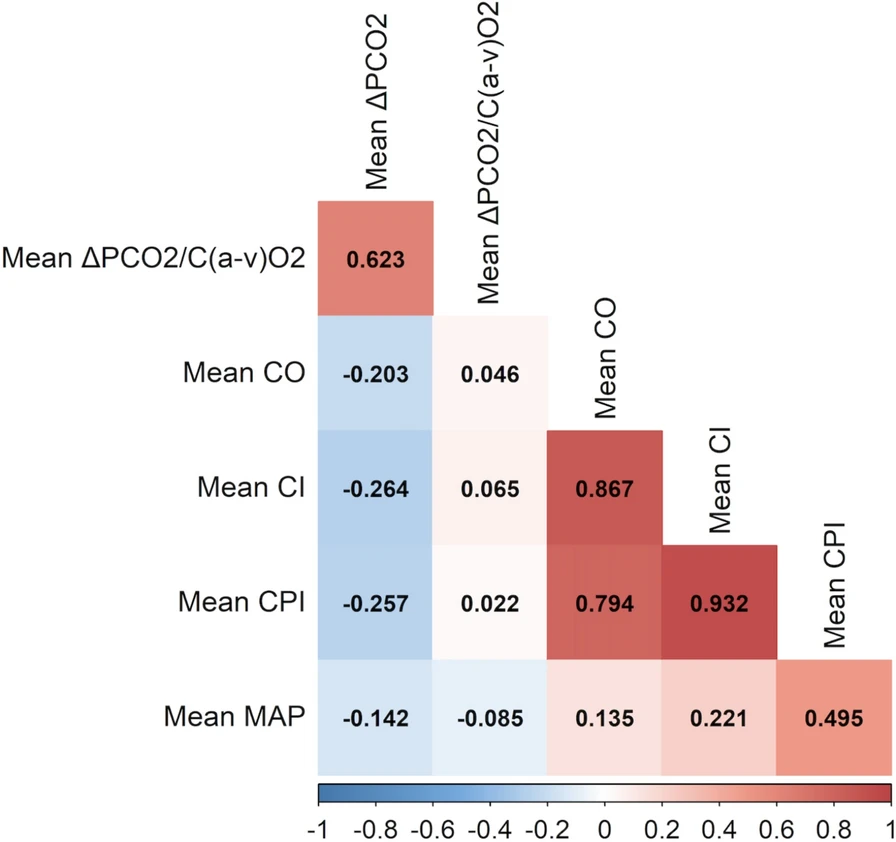
- Biomarker Utility and Challenges: Markers like lactate, base deficit, TEG/ROTEM, syndecan-1, and cytokines (e.g., IL-6, IL-10) help stratify shock severity and guide therapy, though many remain research tools due to limited real-time applicability and standardization.
- Evidence-Based Therapeutics: Clinical data support permissive hypotension, 1:1:1 blood product ratios, and early TXA administration as cornerstones, while therapies like rFVIIa, corticosteroids, and extracorporeal cytokine removal remain investigational with mixed results.
- Future Directions in Shock Management: Precision medicine, AI-driven monitoring systems, mesenchymal stem cell therapy, and endothelial-targeted treatments represent emerging strategies, though integration into practice requires addressing educational, technological, and resource barriers.
Conclusion
Effective management of hemorrhagic shock hinges on timely, phase-specific interventions that address not only perfusion deficits but also the evolving inflammatory and immunologic cascades. While traditional resuscitation strategies remain foundational, emerging therapies and biomarkers hold promise for precision-guided, organ-protective approaches. Future progress will require translational efforts bridging molecular discoveries with practical implementation in diverse clinical settings.
Watch the following video on “Hemorragic Shock,causes ,signs and management , Everything You Need To Know” Dr. Nabil Ebraheim