Abstract
Background: Chronic kidney disease (CKD) and heart failure (HF) are interrelated conditions that exacerbate each other through mechanisms like fluid retention, neurohormonal activation, and inflammation. Red blood cell distribution width (RDW), a measure of red blood cell size variability, has emerged as a potential prognostic marker in HF. This study aimed to assess the prognostic value of RDW in HF patients, both with and without CKD, focusing on all-cause mortality and HF rehospitalizations.
Methods: This observational retrospective study included 171 patients hospitalized for acute decompensated HF in a tertiary university hospital in Greece. Patients were divided into two groups based on their estimated glomerular filtration rate (eGFR), as Group 1 (eGFR < 60 mL/min/1.73 m2) and Group 2 (eGFR ≥ 60 mL/min/1.73 m2). RDW was measured upon admission, and outcomes of interest were all-cause mortality and HF rehospitalizations over a median follow-up period of 6.1 months. Statistical analyses included Kaplan–Meier survival curves, whereas the discrimination traits of RDW were evaluated by constructing receiver operating characteristic (ROC) curves and by calculating the area under the ROC curve (AUC). A p-value <0.05 was indicative of a statistically important result.
Results: Patients in Group 1 (eGFR < 60 mL/min/1.73 m2) were older (80 (73–86) vs. 75 (62–83)) and manifested higher median RDW values (16.6 (15.0–18.8) vs. 15.6 (14.1–17.8)) and received less frequent (57.9% vs. 75%) mineralocorticoid receptor antagonists (MRAs) as compared to those in Group 2 (eGFR ≥ 60 mL/min/1.73 m2). RDW demonstrated better prognostic value in predicting combined mortality and rehospitalization outcomes in Group 2 patients (area under the curve: 0.70; 95% CI (0.62–0.80)) compared to those in Group 1 (area under the curve: 0.53; 95% CI (0.35–0.72)). No statistically significant differences (p = 0.579) were observed in survival between patients with high (≥15%) and low (<15%) RDW values in the overall population, though trends favored worse outcomes with elevated RDW. Similarly, no significant differences (p = 0.374) were observed in survival between patients with high (Group 2) and low (Group 1) eGFR values.
Conclusions: RDW appears to be a meaningful prognostic biomarker for HF patients, particularly in those without CKD. Further multicenter studies are needed to validate its clinical utility and potential for guiding treatment in this high-risk population.
Key Points
- Study Focus: Examined RDW’s prognostic role in HF patients grouped by CKD status (eGFR <60 and ≥60).
- Findings: RDW was a better predictor of combined mortality and HF rehospitalizations in patients with normal renal function (eGFR ≥60).
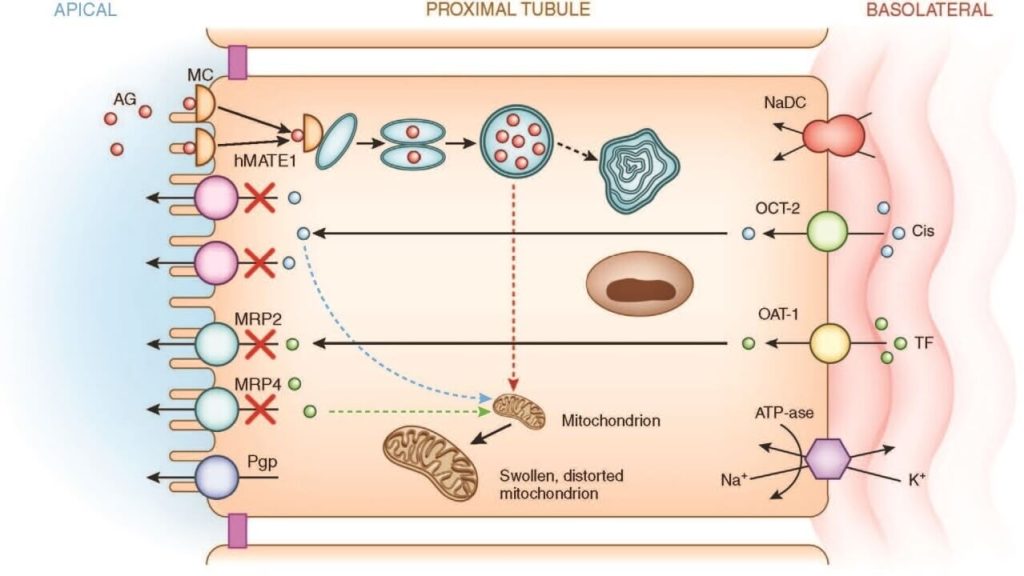
- RDW and CKD: Prognostic value was limited in HF patients with CKD, likely due to heightened inflammation, oxidative stress, and impaired erythropoiesis.
- Patient Data: Patients in the CKD group were older and had higher median RDW values.
- Methodology: Outcomes assessed via Kaplan–Meier survival curves and receiver operating characteristic (ROC) analysis, showing fair discrimination traits for RDW in non-CKD patients (AUC = 0.70).
- Limitations: Small sample size, retrospective design, and lack of granular data on confounders like albumin levels or hepcidin.
- Clinical Implications: RDW could aid in risk stratification for HF patients without renal dysfunction but warrants cautious application in CKD contexts.
- Future Directions: Larger, multicenter studies needed to confirm RDW’s clinical utility in guiding HF management.