Abstract
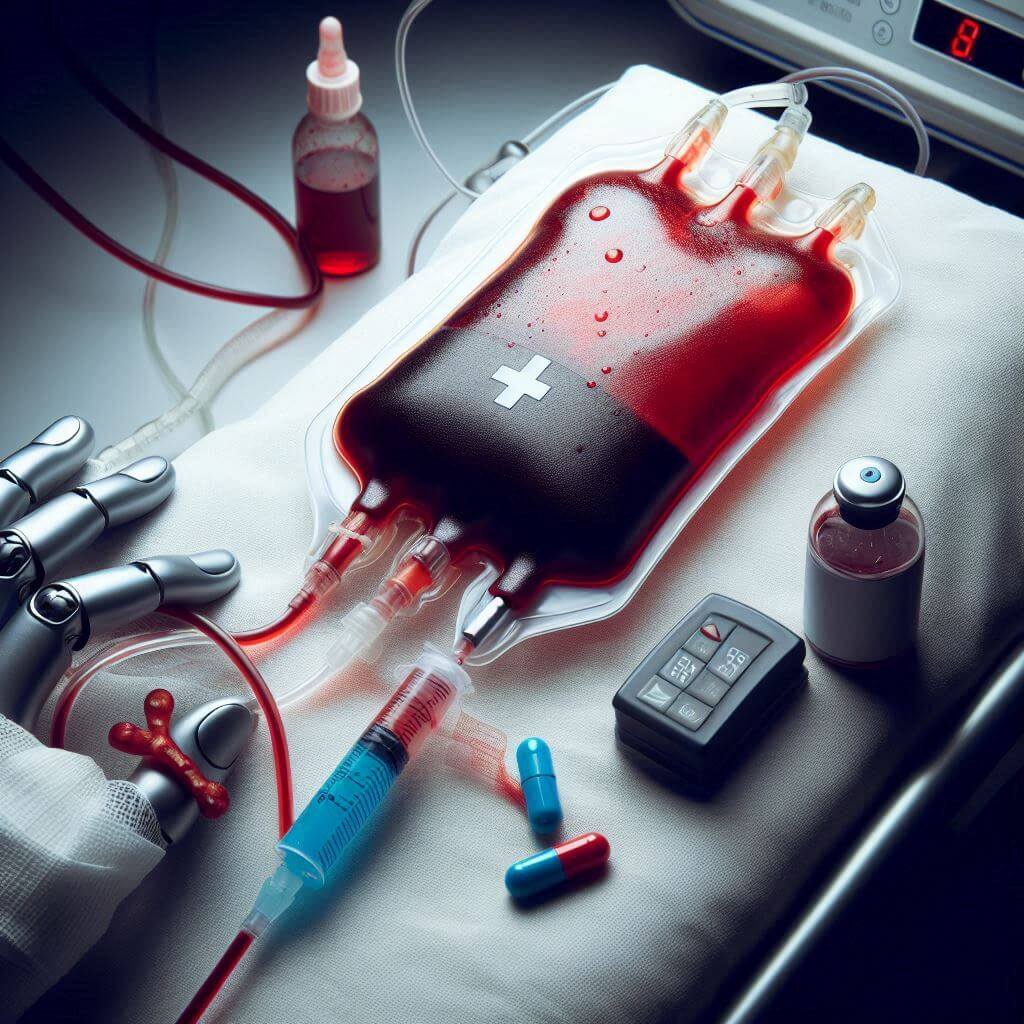
Intraoperative cell salvage (IOCS) allows the collection, treatment, and retransfusion of shed blood from the surgical field and cardiopulmonary bypass (CPB) collector during cardiac surgery. This technique has been shown to reduce the need for allogeneic blood products in many surgical specialties.1
Centrifugation-based IOCS devices enable red blood cell (RBC) reinfusion, whereas platelets and other coagulation factors are largely eliminated during processing.2 Although this technique permits reducing RBC transfusion exposure, it does not reduce the need for allogeneic platelet transfusion.3,4
Knowing the role of platelets in surgical bleeding,5 and considering the risks associated with platelet transfusion,6 the SAME device (i-SEP) was developed to save and wash both RBC and platelets,7 with a recovery rate of 86.1% and 52.4%, respectively.8 The SAME device was developed based on a noncentrifugal recovery of cells from shedded blood, using membrane filtration technology. This technique preserves a higher number of platelets and avoids cell alteration due to centrifugation process.
The SAME Erythrocytes and Platelets Innovative Autotransfusion (SEPIA) registry was created to compare routine cell-salvage solutions with the same device in patients undergoing hemorrhagic surgeries throughout France. Herein we report our pilot experience from the first institution enrolling patients in the SEPIA registry.
