Abstract
Background
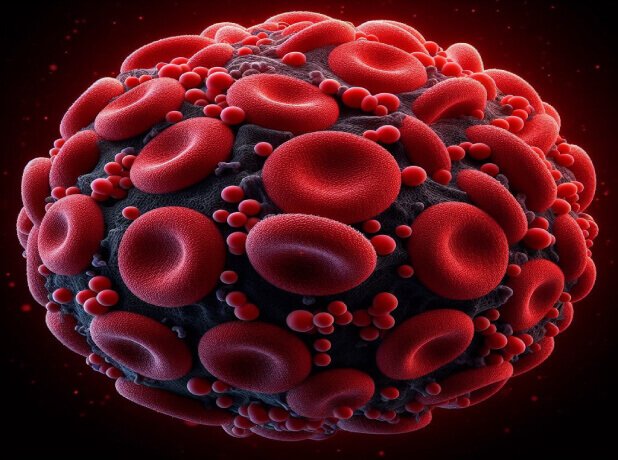
Extracorporeal membrane oxygenation (ECMO) is a life-saving treatment, but carries a high risk of complications such as acute kidney injury (AKI). A contributor to AKI is hemolysis, which induces vasoconstriction and renal tubular cytotoxicity. Here, we have investigated a novel hypothesis that ECMO-induced hemolysis contributes to vascular leakage, edema, microcirculatory perfusion disturbances, and AKI in a rat model.
Methods
Rats were exposed to 75 min of ECMO or a sham procedure as control (n = 8 per group). Hemodynamic, blood gas, and microcirculatory perfusion parameters were monitored throughout the experiment. Renal vascular leakage and edema were determined by dextran leakage (70 kDa) and wet-to-dry weight ratio. Markers of hemolysis, inflammation, endothelial activation and damage, and AKI were assessed using spectrophotometry, ELISA and Luminex.
Results
Initiation of ECMO increased circulating cell-free hemoglobin (CFHb) compared to baseline (4.01 vs. 1.36 OD, p < 0.001). In parallel, ECMO increased circulating levels of TNFα, IL-6, ICAM-1 and angiopoietin-2, whereas levels in the control group remained stable. The number of continuously perfused vessels (4.36 vs. 13.62 vessels/recording, p < 0.001) and the proportion of perfused vessels (PPV; 23.0 vs. 67.4%, p < 0.001) immediately decreased after initiation of ECMO when compared to controls and remained disturbed one hour after weaning from ECMO. Furthermore, NGAL, a marker of kidney injury, in plasma and urine was higher in the ECMO group compared to the controls (respectively 2191 vs. 410 ng/mL, p < 0.001; 1733 vs. 437 ng/mL, p = 0.0059). Wet-to-dry weight ratio showed increased renal edema in the group undergoing ECMO (4.50 ± 0.27 vs. 3.96 ± 0.16, p < 0.001). Moreover, increasing levels of CFHb in plasma were correlated with a decrease in PPV (r=-0.925, p < 0.001) as well as an increase in plasma NGAL (r = 0.895, p < 0.001) in rats on ECMO.
Conclusion
In conclusion, ECMO-induced hemolysis is paralleled by endothelial damage, microcirculatory perfusion disturbances, and kidney injury in a rat model. Our findings suggest that CFHb plays an important role in the pathophysiology of AKI, possibly via endothelial damage. Future studies should clarify the causal relationship between CFHb and endothelial damage, and explore whether targeting CFHb can improve microvascular perfusion and preserve kidney function during ECMO support.
