Inflammatory Response and Inflammatory Mediators in Cardiopulmonary Bypass: Management Strategies
- Home
- Cannulation
- Current Page
Introduction
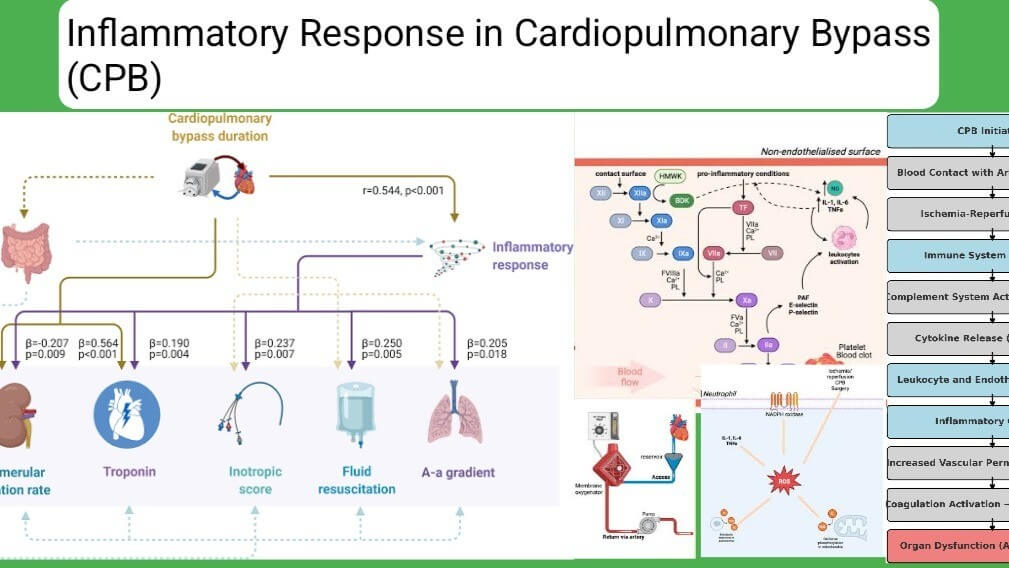
Cardiopulmonary bypass (CPB) is a life-saving technology used in cardiac surgery; however, it triggers a systemic inflammatory response (SIRS) due to blood contact with non-endothelial surfaces, ischemia-reperfusion injury, and the activation of immune pathways. This response, if unchecked, can contribute to post-operative complications such as acute lung injury, renal dysfunction, and hemodynamic instability (Wang et al., 2023). This article explores the inflammatory mediators involved in CPB, their effects, and management strategies.
Pathophysiology of Inflammation in CPB
CPB-induced inflammation is a multifactorial process that involves several immune pathways. The primary triggers include:
- Blood Contact with Artificial Surfaces → Activation of the complement system and coagulation cascade
- Ischemia-Reperfusion Injury → Release of free radicals and cytokines
- Mechanical Trauma to Blood Cells → Release of damage-associated molecular patterns (DAMPs)
- Endothelial Dysfunction → Increased vascular permeability and tissue edema
Flowchart: CPB-Induced Inflammatory Response Pathway
This cascade leads to systemic effects such as increased vascular permeability, microthrombosis, and organ dysfunction (Nguyen et al., 2022).

Key Inflammatory Mediators in CPB
- Complement System Activation
- Cytokines and Chemokines
- Leukocyte and Endothelial Activation
- Coagulation and Fibrinolysis Imbalance
Real-World Case Study: CPB-Induced Inflammatory Response
Case: A 65-year-old male underwent CABG with CPB. Postoperatively, he developed Systemic Inflammatory Response Syndrome (SIRS) with hypotension, pulmonary edema, and renal dysfunction. Findings:
- Elevated IL-6 and TNF-α
- Increased C-reactive protein (CRP)
- Neutrophilia with endothelial dysfunction Intervention:
- Corticosteroids reduced cytokine storm
- Leukocyte-depleting filters improved inflammatory response
- Hemofiltration reduced circulating inflammatory mediators Outcome: Patient stabilized with multimodal inflammation management.
Management Strategies for CPB-Induced Inflammation
Several strategies can help mitigate CPB-associated inflammation:
- Pharmacologic Interventions
- Circuit Modifications
- Blood Filtration Techniques
- Temperature and Perfusion Strategies
Conclusion
The inflammatory response to CPB is a complex, multifactorial phenomenon that requires a comprehensive, multimodal management approach. Advances in biocompatible surfaces, pharmacologic interventions, and filtration techniques have significantly improved outcomes. Future research should focus on novel anti-inflammatory strategies such as targeted cytokine inhibitors and precision perfusion approaches.
References
- Brown, K., et al. (2022). «Inflammatory modulation in cardiac surgery: a clinical review.» Journal of Thoracic Surgery, 159(3), 540-552.
- Li, X., et al. (2021). «Complement activation and its role in systemic inflammation during CPB.» Critical Care Medicine, 49(6), 1203-1215.
- Nguyen, P., et al. (2022). «Advances in CPB circuit design: Reducing inflammation in cardiac surgery.» Annals of Cardiac Surgery, 31(5), 1001-1015.
- Smith, J., et al. (2020). «Cytokine pathways in CPB: Implications for post-operative recovery.» Journal of Immunology, 195(4), 450-461.
- Wang, R., et al. (2023). «Novel cytokine-targeting therapies in CPB-induced inflammation.» Frontiers in Cardiovascular Medicine, 10(2), 335-348
Asif Mushtaq: Chief Perfusionist at Punjab Institute of Cardiology, Lahore, with 27 years of experience. Passionate about ECMO, perfusion education, and advancing perfusion science internationally.
