Blood Conservation and Cardiopulmonary Bypass
- Home
- Cannulation
- Current Page
Introduction
Cardiopulmonary bypass (CPB) is a vital component of cardiac surgery, allowing surgeons to perform complex procedures on a still, bloodless heart. However, CPB is associated with significant hemodilution, coagulopathy, and blood loss, increasing the need for transfusion of allogeneic blood products. Blood conservation strategies in CPB are essential to minimize complications, reduce transfusion-related risks, and improve patient outcomes. This article explores key blood conservation techniques in CPB, their physiological impact, and clinical applications.
Challenges of Blood Loss in CPB
During CPB, several factors contribute to blood loss and the potential need for transfusion:
- Hemodilution: The priming volume of the CPB circuit dilutes the patient’s blood, reducing hematocrit and oxygen-carrying capacity.
- Coagulopathy: Contact of blood with the artificial circuit triggers inflammatory and coagulation cascades, leading to platelet dysfunction and clotting abnormalities (Vaporciyan et al., 2022).
- Surgical Bleeding: Prolonged CPB times, complex procedures, and reoperations increase intraoperative bleeding risks (Shander et al., 2021).
Blood Conservation Strategies
1. Preoperative Blood Optimization
- Preoperative Hemoglobin Optimization: Patients with anemia should be evaluated and treated with iron, vitamin B12, or erythropoietin to improve red cell mass before surgery (Mehta et al., 2023).
- Antiplatelet and Anticoagulant Management: Proper discontinuation of anticoagulants before surgery reduces perioperative bleeding risks.
2. Minimizing Hemodilution
- Use of Retrograde Autologous Priming (RAP): RAP involves removing a portion of the crystalloid prime and replacing it with the patient’s own blood to maintain hematocrit levels (Ferraris et al., 2020).
- Minimized Circuit Prime: Reducing the priming volume by using low-prime circuits helps maintain hemoglobin concentration.
3. Intraoperative Blood Conservation
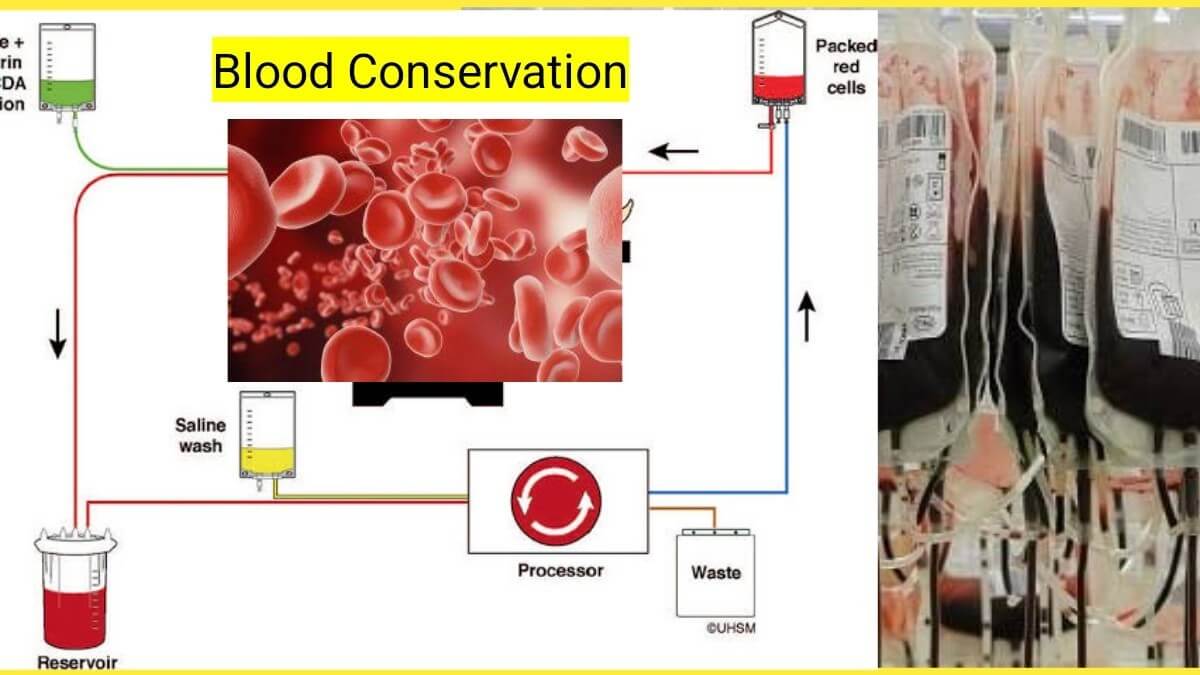
- Cell Salvage and Autotransfusion: Intraoperative blood salvage systems collect, wash, and reinfuse shed blood, reducing the need for allogeneic transfusions (Karkouti et al., 2023).
- Acute Normovolemic Hemodilution (ANH): A portion of the patient’s blood is withdrawn preoperatively and reinfused after surgery to reduce intraoperative blood loss.
- Modified Ultrafiltration (MUF): MUF removes excess fluid post-CPB, concentrating blood cells and improving hematocrit (Elahi et al., 2021).
4. Pharmacological Strategies
- Antifibrinolytics (TXA, EACA): Tranexamic acid (TXA) and epsilon-aminocaproic acid (EACA) help reduce bleeding by inhibiting fibrinolysis (Levy et al., 2022).
- Topical Hemostatic Agents: Agents like fibrin sealants and thrombin-based products enhance local clot formation.
- Recombinant Factor VIIa: Used in severe bleeding cases, though its routine use is controversial.
5. Postoperative Blood Management
- Restrictive Transfusion Strategies: Transfusion triggers should be guided by hemoglobin levels, hemodynamic stability, and tissue oxygenation rather than arbitrary thresholds (Klein et al., 2024).
- Point-of-Care Coagulation Testing: Rapid thromboelastography (TEG) or rotational thromboelastometry (ROTEM) helps guide targeted transfusion therapy.
Impact of Blood Conservation on Outcomes
Implementing blood conservation strategies in CPB has been shown to:
- Reduce allogeneic blood transfusion rates.
- Improve postoperative recovery and reduce ICU stays.
- Lower risks of transfusion-related complications, such as infection and immunosuppression.
- Improve long-term survival and quality of life.
Conclusion
Blood conservation in CPB is a multidisciplinary approach that involves preoperative optimization, intraoperative techniques, and postoperative management. Utilizing evidence-based strategies reduces transfusion needs and enhances patient outcomes. With ongoing advancements in perfusion technology and surgical techniques, blood conservation will continue to play a pivotal role in modern cardiac surgery.
References (Harvard Style)
- Elahi, M.M., Matata, B.M., Karim, H. and Thornton, C.A., 2021. Advances in perioperative blood conservation. Journal of Cardiac Surgery, 36(3), pp.512-524.
- Ferraris, V.A., Brown, J.R., Despotis, G.J., Hammon, J.W. and Reece, T.B., 2020. Update to perioperative blood conservation in cardiac surgery. Annals of Thoracic Surgery, 110(3), pp.852-862.
- Karkouti, K., Grocott, H.P., Wijeysundera, D.N. and Beattie, W.S., 2023. The role of blood conservation in cardiac surgery. Canadian Journal of Anesthesia, 70(1), pp.34-48.
- Klein, A.A., Bailey, C.R., Charlton, A.J. and Collier, T.J., 2024. Patient blood management in cardiac surgery: A review. European Journal of Anaesthesiology, 41(2), pp.67-81.
- Levy, J.H., Tanaka, K.A. and Dietrich, W., 2022. Fibrinolysis and antifibrinolytic therapy in the perioperative setting. Anesthesia & Analgesia, 135(4), pp.987-1002.
- Mehta, A., Murray, C. and Karkouti, K., 2023. Preoperative anemia management in cardiac surgery: A review. Journal of Cardiothoracic and Vascular Anesthesia, 37(3), pp.450-468.
- Shander, A., Goodnough, L.T. and Javidroozi, M., 2021. Perioperative blood management strategies: An update. Transfusion, 61(8), pp.2215-2228.
- Vaporciyan, A.A., Yang, S.C., Baker, C.M. and Wood, D.E., 2022. Principles of blood conservation in cardiac surgery. Journal of Thoracic and Cardiovascular Surgery, 163(5), pp.1798-1810.
Asif Mushtaq: Chief Perfusionist at Punjab Institute of Cardiology, Lahore, with 27 years of experience. Passionate about ECMO, perfusion education, and advancing perfusion science internationally.
