Biocompatible and Miniaturized Cardiopulmonary Bypass Circuits: Shaping the Future of Cardiac Surgery
- Home
- Cannulation
- Current Page
Introduction
Cardiopulmonary bypass (CPB) is fundamental to modern cardiac surgery, allowing surgeons to perform complex procedures on a still and bloodless heart. However, traditional CPB systems are associated with complications such as systemic inflammatory responses, coagulation abnormalities, and organ dysfunction due to the extensive blood contact with foreign surfaces (Ranucci et al., 2009). The development of biocompatible and miniaturized CPB (mCPB) circuits addresses many of these issues, improving outcomes, especially in neonates and high-risk patients.
Conventional CPB Circuits and Their Limitations
Traditional CPB circuits involve large surface areas, open reservoirs, and significant priming volumes. These features increase blood exposure to non-physiological surfaces, leading to hemolysis, systemic inflammation, and coagulation disturbances (Wiesenack et al., 2000). Hemodilution from large priming volumes further contributes to the need for blood transfusions, increasing risks of infection and transfusion-related reactions (Ranucci et al., 2009).
Design and Advantages of Miniaturized CPB Circuits
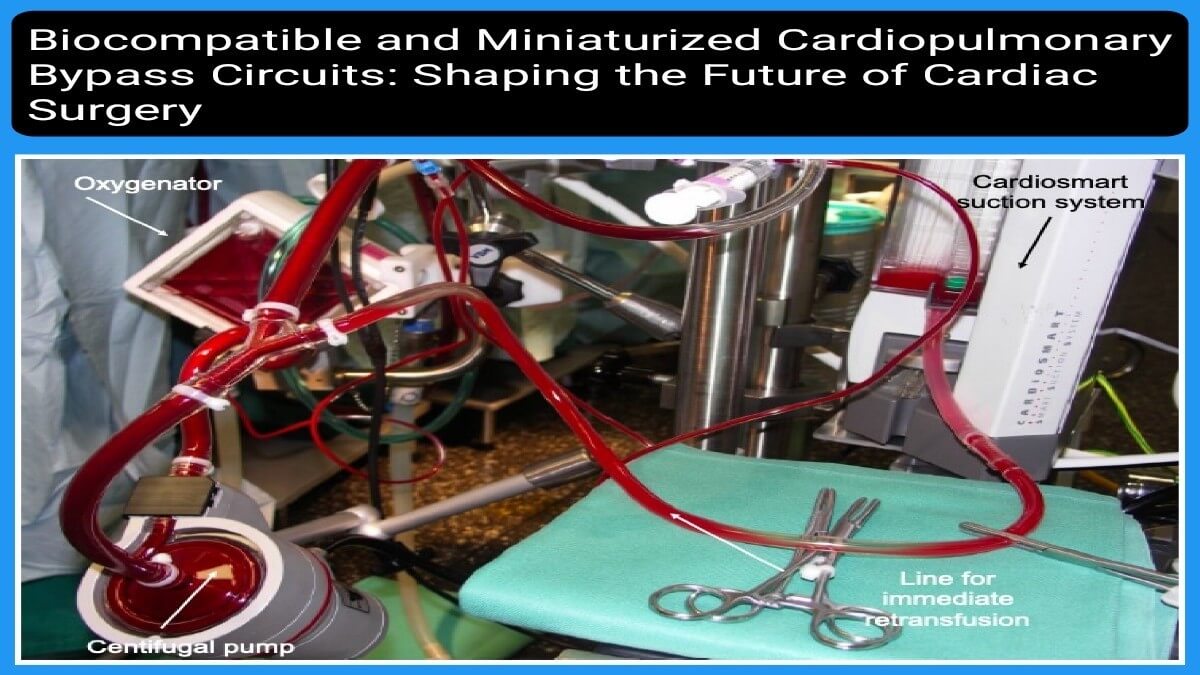
Miniaturized CPB circuits are designed to overcome the limitations of conventional systems. They feature shorter tubing, closed-loop systems without open reservoirs, and significantly reduced priming volumes (Koster et al., 2008). These designs decrease the blood-contact surface area and reduce air–blood interface, mitigating systemic inflammatory responses.
Clinical studies demonstrate that miniaturized circuits reduce transfusion requirements, lower levels of inflammatory cytokines, and improve hemodynamic stability (Sakamoto et al., 2011). These outcomes are especially critical in pediatric populations where physiological reserves are limited (Boeken et al., 2005).
Biocompatibility Coatings and Their Impact
In addition to miniaturization, improving biocompatibility of circuit components has been a major innovation. Coatings such as heparin, phosphorylcholine (PC), and poly-2-methoxyethylacrylate (PMEA) reduce the activation of platelets and the complement system (Wiesenack et al., 2000; Ranucci et al., 2009).
Heparin-coated circuits inhibit thrombin formation and platelet activation, while PC coatings mimic the phospholipid membrane of red blood cells, reducing protein adsorption and inflammatory responses. PMEA coatings provide a hydrophilic interface that resists cell and protein adhesion (Boeken et al., 2005).
Clinical Advantages
The combination of miniaturized and biocompatible CPB circuits leads to a wide range of clinical advantages:
- Reduced systemic inflammation (Ranucci et al., 2009)
- Decreased need for blood transfusions (Koster et al., 2008)
- Shorter ICU and hospital stays (Sakamoto et al., 2011)
- Improved renal and pulmonary function postoperatively (Boeken et al., 2005)
In pediatric surgery, these benefits are magnified due to smaller blood volumes and heightened vulnerability to inflammation and hemodilution (Sakamoto et al., 2011).
Challenges and Considerations
Despite their benefits, miniaturized and biocompatible CPB systems present challenges. These include:
- Higher initial costs due to specialized materials and coatings
- Technical complexity requiring specialized training
- Not all patients are ideal candidates due to anatomical or procedural limitations (Ranucci et al., 2009)
Nevertheless, ongoing innovation and broader adoption are expected to overcome many of these hurdles.
Future Directions
Future trends in CPB include:
- Tailored perfusion strategies based on patient-specific physiology, enhancing the precision of circulatory support.
- Development of advanced biocompatible materials, including next-generation surface coatings to further reduce inflammatory responses and clotting risks.
- Integration of compact and portable CPB systems for use in emergency and minimally invasive procedures.
- Improved real-time perfusion monitoring tools that enhance safety through direct human control and feedback mechanisms.
- Enhanced training protocols and simulation models for perfusionists to ensure safe adoption of miniaturized systems.
These innovations aim to increase safety, broaden applicability, and support the evolution of more personalized and less invasive cardiac surgery techniques.
Conclusion
Biocompatible and miniaturized CPB circuits represent a major step forward in perfusion technology. By reducing inflammatory responses, minimizing transfusion needs, and improving patient outcomes, they are reshaping the future of cardiac surgery. As these technologies become more widespread, they hold promise for safer and more effective cardiovascular interventions.
Asif Mushtaq: Chief Perfusionist at Punjab Institute of Cardiology, Lahore, with 27 years of experience. Passionate about ECMO, perfusion education, and advancing perfusion science internationally.
